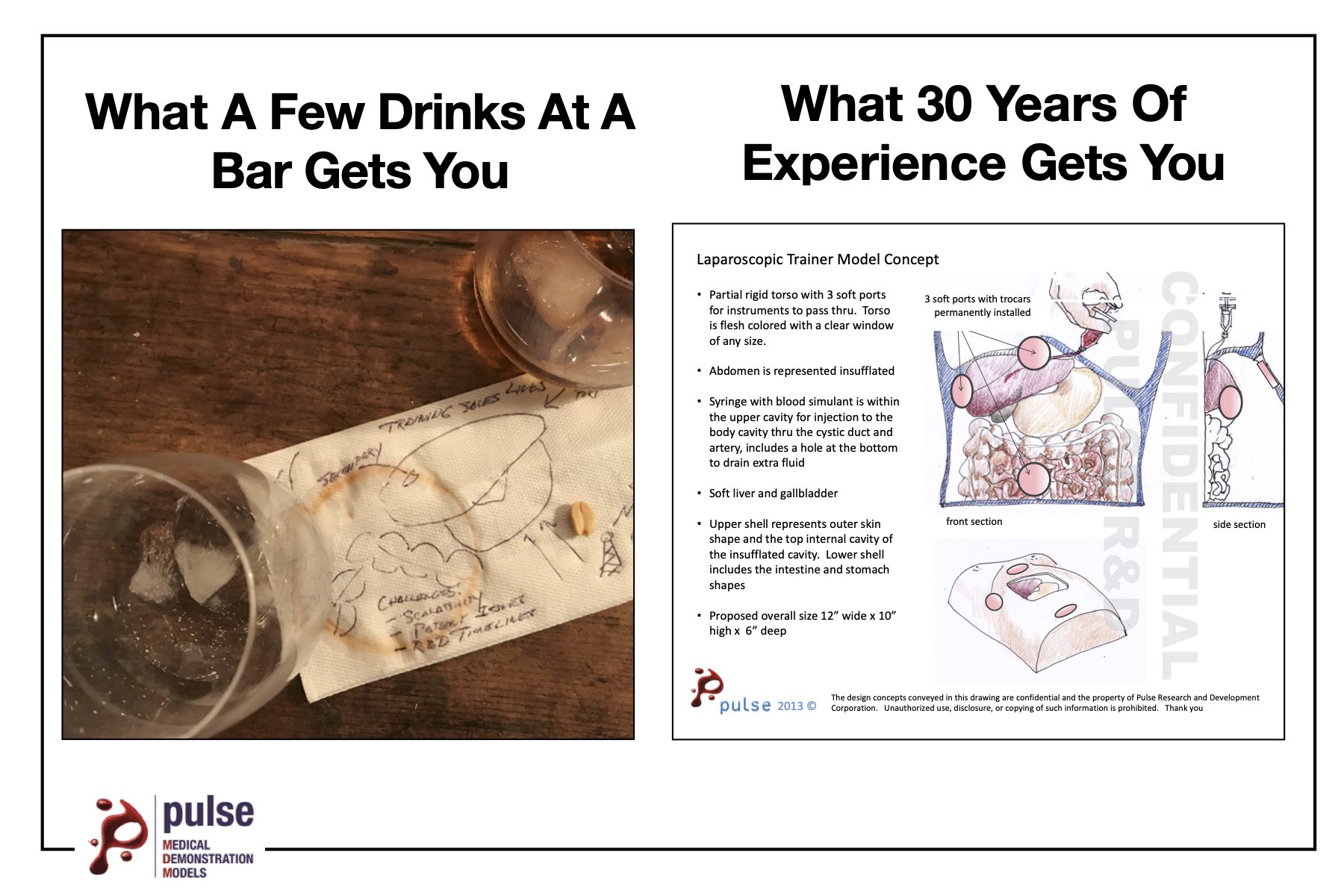
When Models Marry Cadavers
How Hands-On Models and Cadaver Labs Create the Best Experience for Training Medical Professionals
Cadavers have been used for medical training and research since the 13th century. Over the past several hundred years, cadavers have undoubtedly enhanced the medical profession and allowed a mode of training that garnered a realistic and generally reproducible training experience. As technology has progressed exponentially over the years, cadaver labs have been joined by hands-on anatomical models to enhance the training of clinicians, residents, and medical students. To this day, cadaver labs continue to be an extremely effective mode of training but are now joined on the throne of gold-standard medical training by hands-on models.
Cadaver Labs: The Pros
Cadaver labs have stood the test of time. Just ask any patient-facing medical provider or medical student if they’ve worked with a cadaver at least once, and nearly all will tell you that they have.
Although rather eerie, let’s face it, cadaver labs are cool. They provide us with a true-to-scale way to learn about the human body. Along with that, they provide the ability for healthcare providers to train and learn their craft without the risk of negative outcomes.
With the obvious fact that cadavers lack the blood flow of a living patient, they are all tested for pathogens (including Covid) and must meet certifications that the required tissues are present before they can be utilized by their intended clientele.
Cadaver Labs: The Drawbacks
Just as the positive aspects of cadaver labs should be recognized, it is equally important to weigh the shortcomings of this long-standing method of training. First is the availability concern. Unfortunately, cadaver availability for medical and scientific purposes is extremely limited when compared to the need. And for those that do become available, there’s only ever the opportunity for one ‘first cut’ per body structure. This often leaves a room full of clinicians or students standing around watching as one or a few people practice a skill that will soon become unavailable for anyone else to practice.
Even though nothing can be more real than actual human tissue, cadavers are also typically left with features that aren’t particularly realistic. This may sound a bit morbid, but consider that after a person dies, their tissues, organs, and systems no longer have the amazingly orchestrated processes occurring that allow humans to be human. For anyone who has ever been in a cadaver lab, this explains the impossible-to-ignore aroma of embalming chemicals.
Although chemicals can preserve the cadaver from decaying externally, these same chemicals affect the external tissue properties of the cadaver. Additionally, it is impossible to prevent the natural events that occur internally after death. Even with a short turnaround time, many of the internal and external tissue properties of the cadaver will no longer resemble that of the living patients clinicians will work with.
The New Age
With the incredible technology we have available to us today, medical device manufacturers, medical salespeople, and clinical trainers can help fill in the cracks that cadaver labs leave behind. Nearly all the shortcomings of cadaver labs outlined above can be supplemented by hands-on anatomical models.
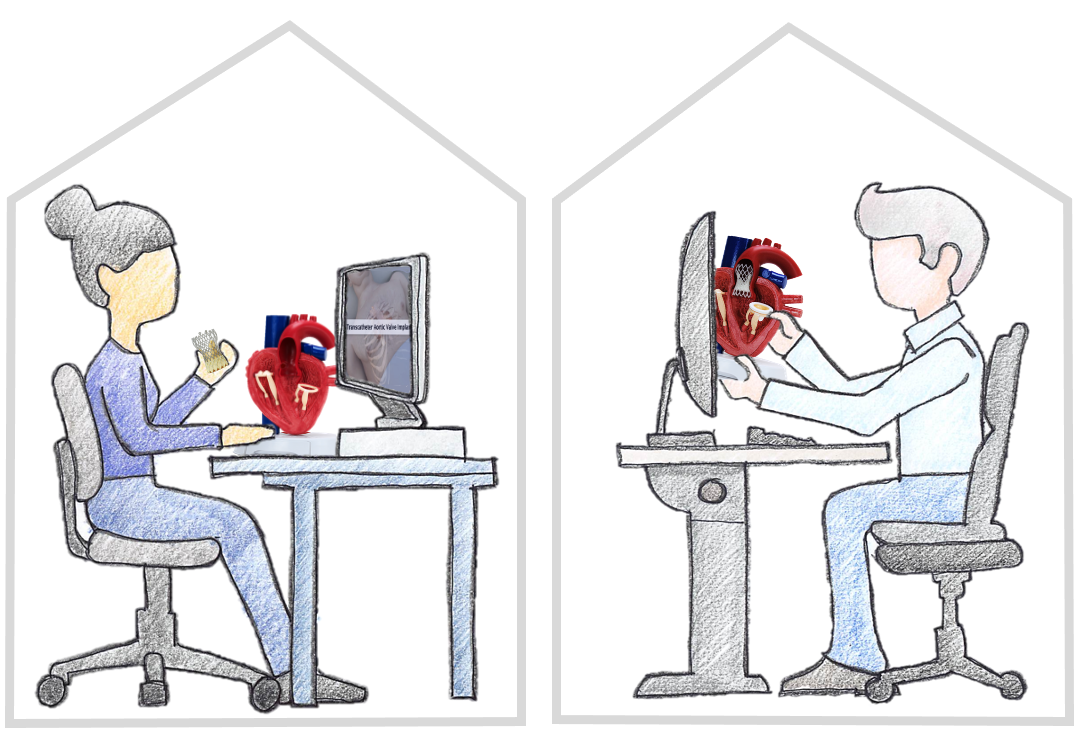
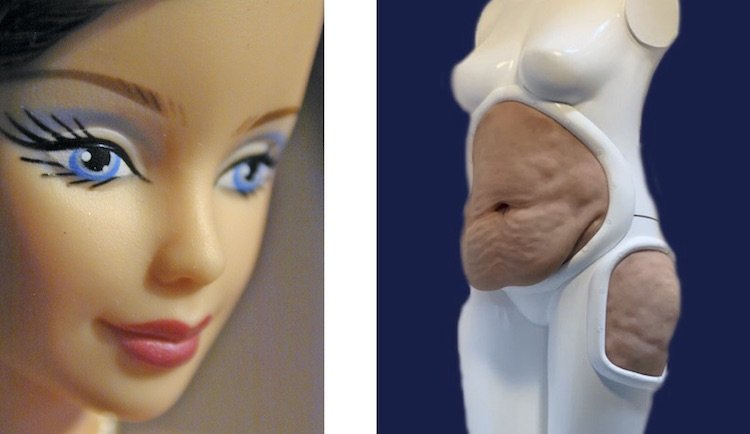
Today, hands-on models are being adopted as either an alternative or supplement to cadavers by some organizations but continue to be overlooked by others. The reasons for those that overlook the models vary but generally comes down to either a lack of awareness of the versatility of hands-on models or a belief that models do not provide a high-quality, realistic experience. In reality, models are fully customizable for the client, ensuring they are built to the specific standards necessary to provide the exact training experience needed for their healthcare providers.
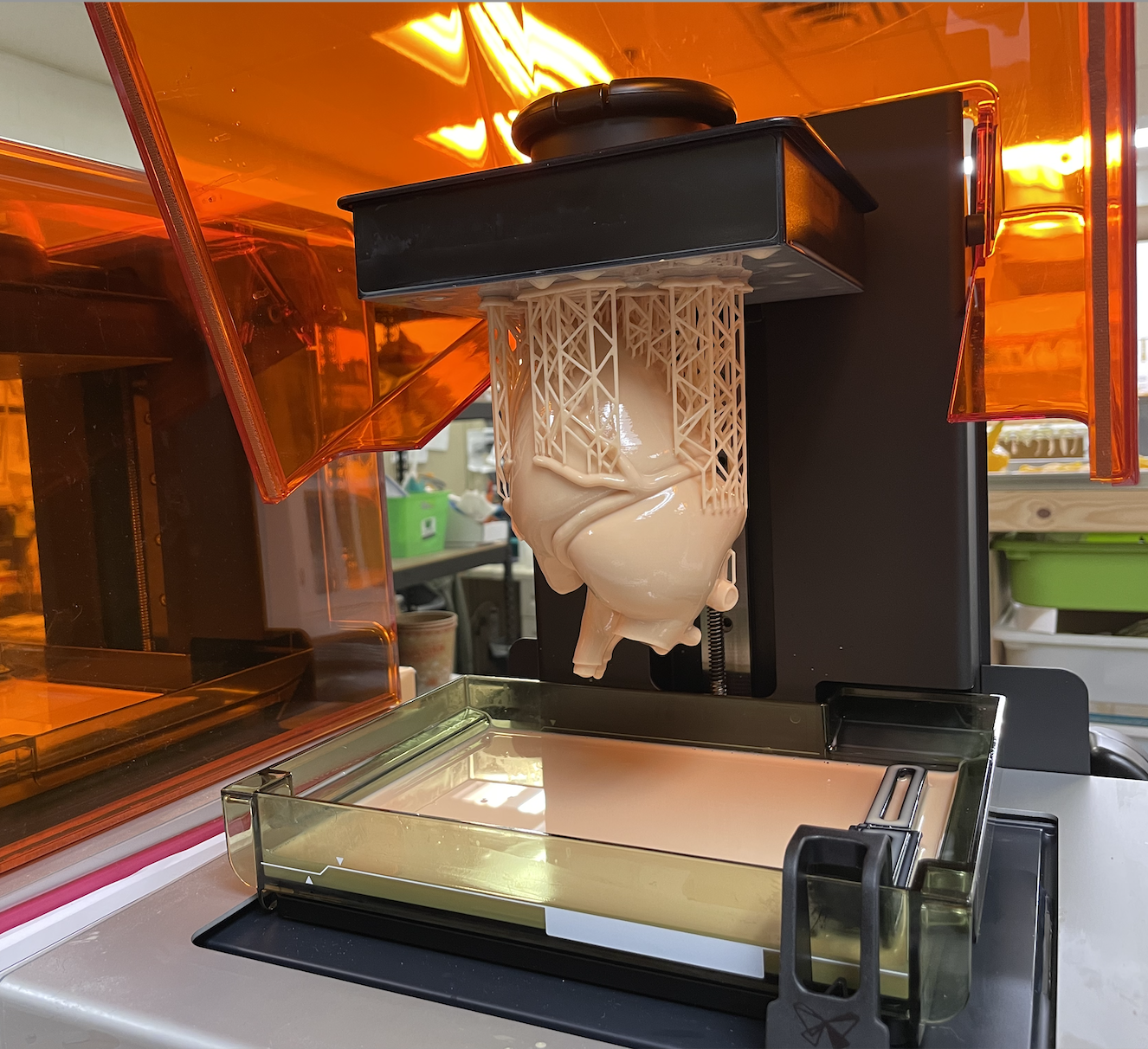
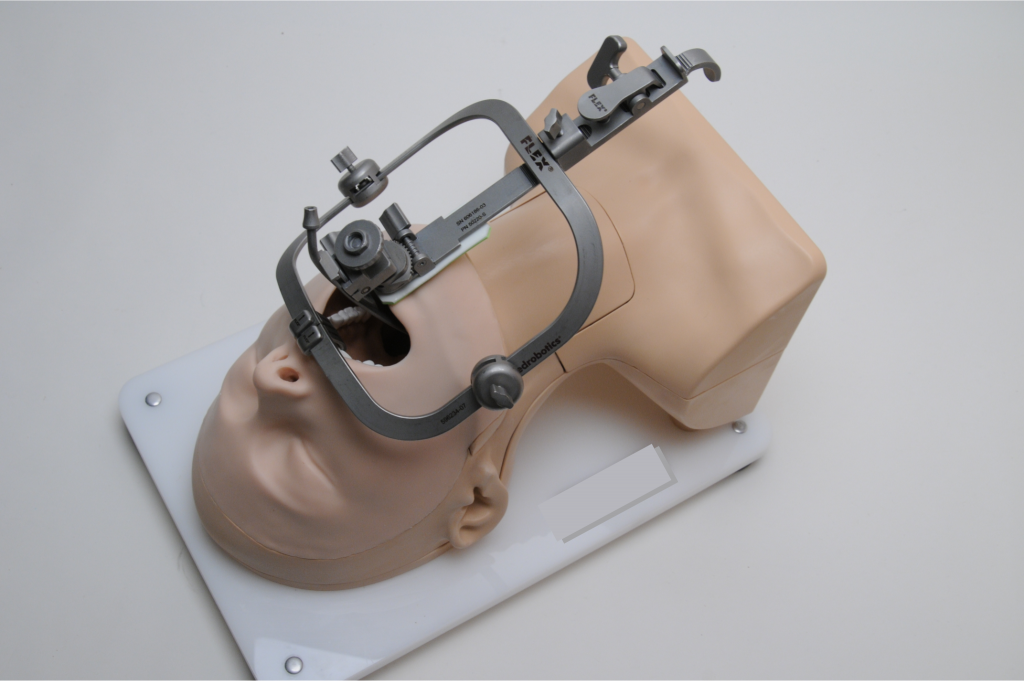
As outlined in last month’s blog post, hands-on models are designed and cast with extreme dedication to replicate specific clinical scenarios. The design, materials, colors, and transparency can all be altered until they meet the exact specifications of the client. This eliminates the issue found with cadaver labs where the cadaver’s structures no longer resemble a realistic feel or durability of a living patient.
More importantly, the “one first cut” problem is completely eliminated with cleverly designed consumables. As discussed above, the limited availability of cadavers often leaves many students and clinicians in a position where they are doing more observing of their peers than actually performing incisions and surgical techniques themselves. Custom-designed hands-on models provide easily replaceable parts in any quantity needed to ensure that every surgeon can make that first cut to receive the proper training and experience needed for proficiency and then utilize cadavers if necessary to perfect the technique on human tissue. This is a telling example of how cadaver labs and hands-on models can supplement one another to provide the best training experience for clinicians and students.
Cost Comparison
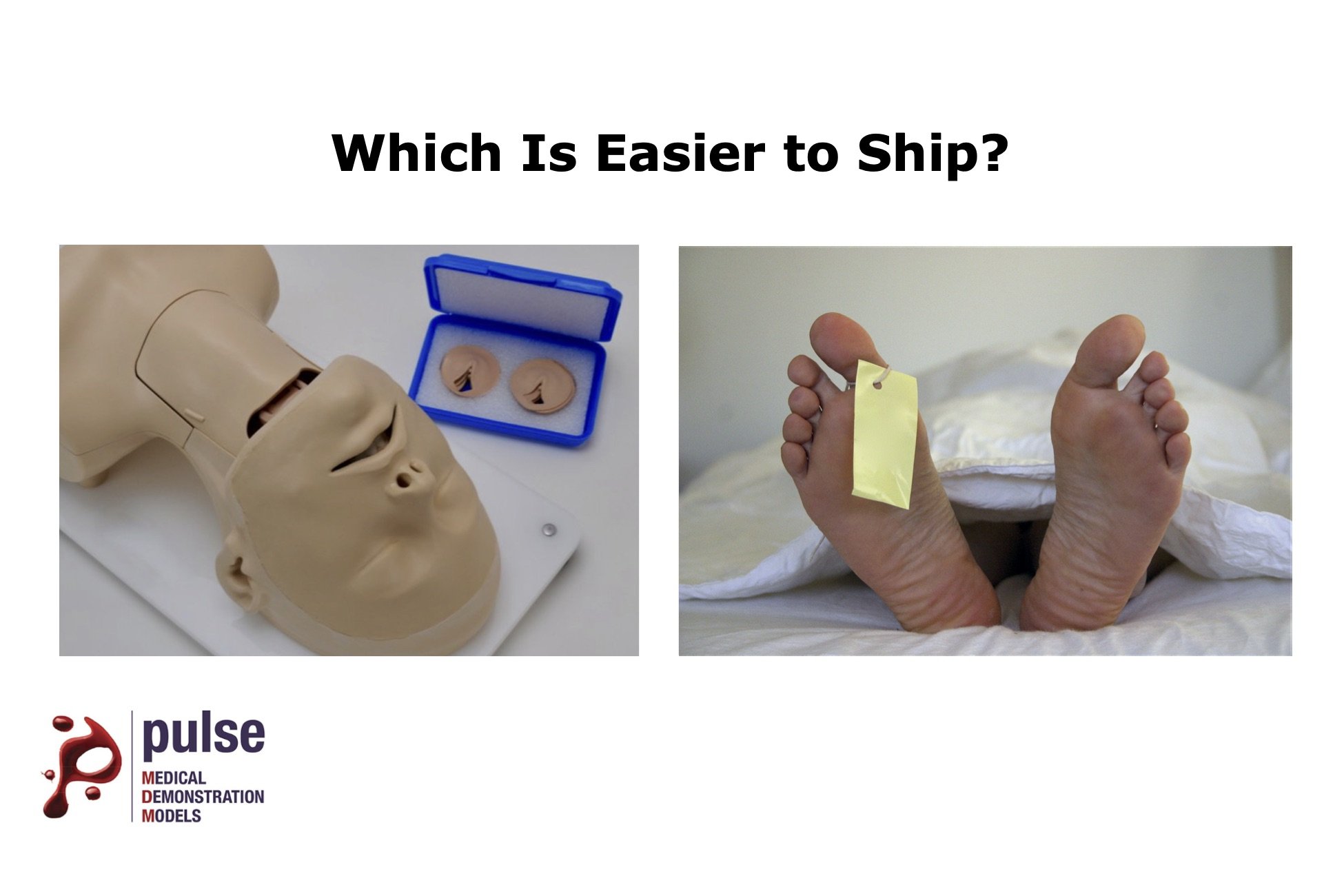
From the perspective of a healthcare organization, the level of reusability and transportability that a model provides means significant cost savings over the long term by eliminating nearly all the recurring costs necessary for cadaver labs. That’s, of course, not to say that both options don’t have their associated costs. A general breakdown of the costs of each looks like this:
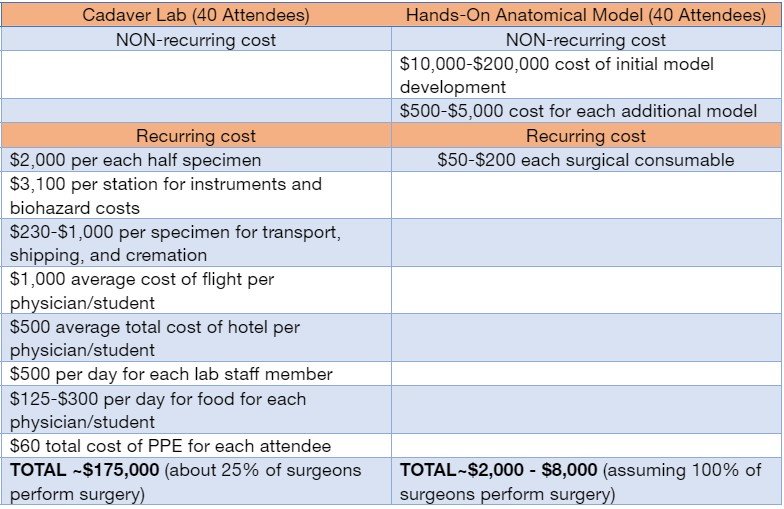
Although both cadaver labs and hands-on models require initial costs, the savings from the lack of recurring costs of hands-on models make the “break-even” point quickly realized.
Cadavers and hands-on models both clearly have their place in medical/surgical training. With healthcare organizations aiming to remain as profitable as possible while simultaneously ensuring their providers can access the highest level of training for improved patient outcomes, this is where the skill and knowledge of medical device manufacturers, medical device salespeople, and clinical trainers truly comes into play. Based on the outlined benefits of hands-on models, it is easy to see how discussing this option with healthcare organizations creates some obvious selling points. In addition to what has been outlined above, note the following:
Hands-on anatomical models provide the following benefits and selling points for your clients:
- Able to be mono or bipolar ablated, lasered, stapled, injected, dissected, debrided, and cut
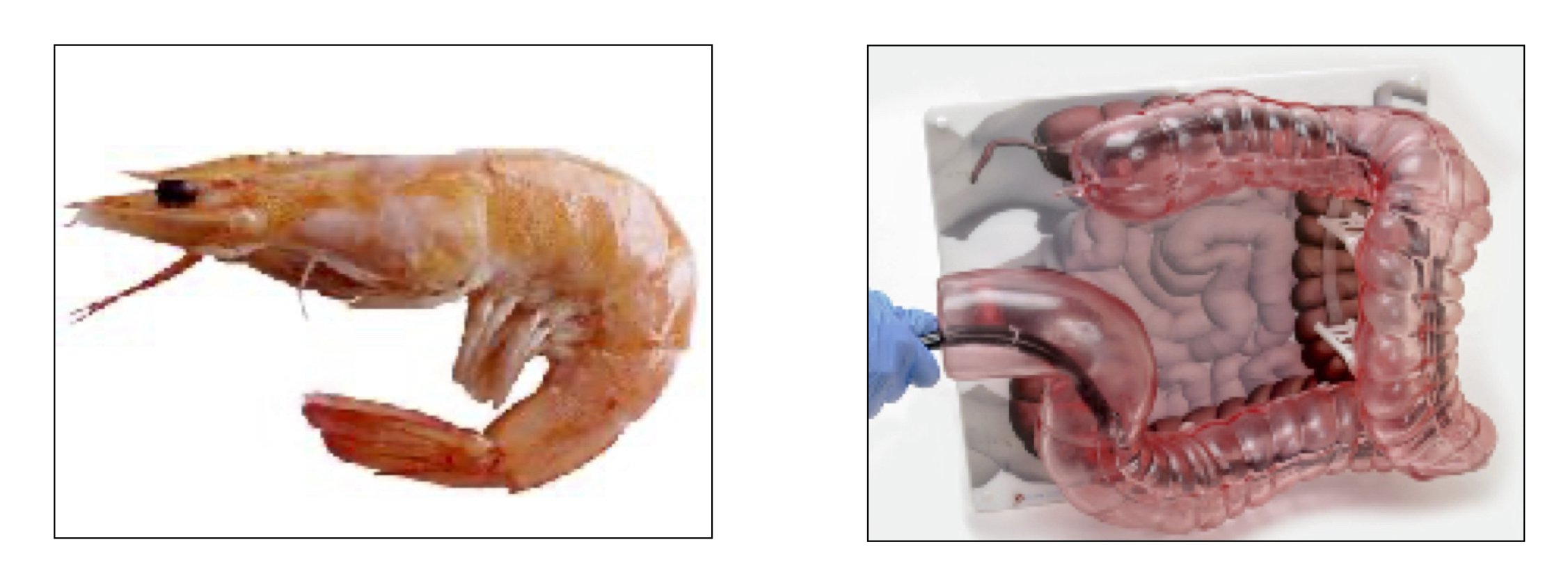
- Infinite custom pathologies that cadavers never have
- Unlimited anatomical variation
- Nearly zero recurring costs once the development and unit costs are covered
- No team required to set up off-site cadaver training
- No team required to make travel arrangements for clinicians
- No clinician travel, lodging, meal, or entertainment costs
- No lab rental costs
- No lab technician costs
- No cadaver shipping costs
- No surgical instrument sterilization
- No cadaver disposal costs
- Training the entire clinical staff as opposed to just the main surgeon by meeting your clients at their locations with a portable model with replaceable parts.
- Consistent and repeatable experiences. Every surgeon gets to make the 1st cut using low-cost, easily replaceable surgical inserts.
- Increased training opportunities since the model can be used and set up without a lab and can be done anywhere (like a hotel conference room).
More training sessions = more mastery.
More mastery = more confidence in your device/procedure.
More confidence = increased surgeon adoption of your procedure.

Wrap-Up
Allowing every surgeon to make the first cut and to hone their skills with a wide range of pathologies and anatomical variance is essential for the safety of the patients whose lives are in their hands every day. By using models as precursors to cadaver labs or in tandem with cadavers, medical students, residents, and clinicians new to a particular type of procedure gain the repetition and muscle memory necessary to perfect their skills, so they have the confidence and buy-in of a technique much more quickly. These models can then be used within patient appointments to ensure the patient has a clear understanding of what is involved in their specific procedure. Getting clinicians to this point of confidence and mastery requires an important role from medical device manufacturers and clinical trainers. The success of your mission comes from the success the surgeons have with their patients.
Pulse Medical Demonstration Models – Making Dreams Come True
When you’re in the model-making business, it’s a true joy to help our clients find the perfect solutions to their greatest challenges. Because our models are customized exactly for your need, we are a huge game-changer for those who need quality models. Contact us today to see how we can help you!